This article is a continuation of a story published here.
“I get a Hollywood wax every 3-4 months. In between that, I use Veet down there.”
That was my manicurist. She pointed towards her thighs with a nail file and then went back to restoring my cuticles.
“In fact, I’ve even gotten my boyfriend to Veet with me.”
“Your…your boyfriend chemically creams his balls?”
“Yeah,” she laughed. “It’s quite nice. He enjoys having smooth balls now. Usually, we smoke a hookah in the bathroom and make an afternoon of it.”
I don’t know why people tell me these things, and I certainly don’t know how we got on the topic of this woman’s pubic grooming habits, but soon our conversation migrated to birth control – a topic that made her feel sad. Not because she didn’t believe in it; but because she was having such a hard time finding the right one for her.
“I had the implant for looong time.” Then she leaned in and whispered behind her mask and the plexiglass barrier between us. Was she about to tell me something more secretive/personal than her boyfriend’s bare balls? “You don’t want to know how much weight I gained! Now I’m taking the shot. I have one child – a boy. And I don’t want any more.”
“I hear you. I have four and I certainly don’t want any more!”
“You look good for having four kids.”
“Thanks,” I said. “But I know what you mean about the weight gain. I was on the pill for many years and I still haven’t lost all the weight.”
I didn’t share my bias against the shot with her. One of my best friends died in 2002 from complications with the birth control shot. Blood clots are one of the possible side effects, and she developed one in her brain. We watched her life slip away and felt her feet turn to ice when they took her off the ventilator. To say it was traumatic is an understatement. I shared none of this with Chantel*, but encouraged her to keep researching options that would help her reach her personal health and family planning goals. It was that conversation that sparked my interest in, and curiosity about IUDs, which I would later ask my healthcare provider about.

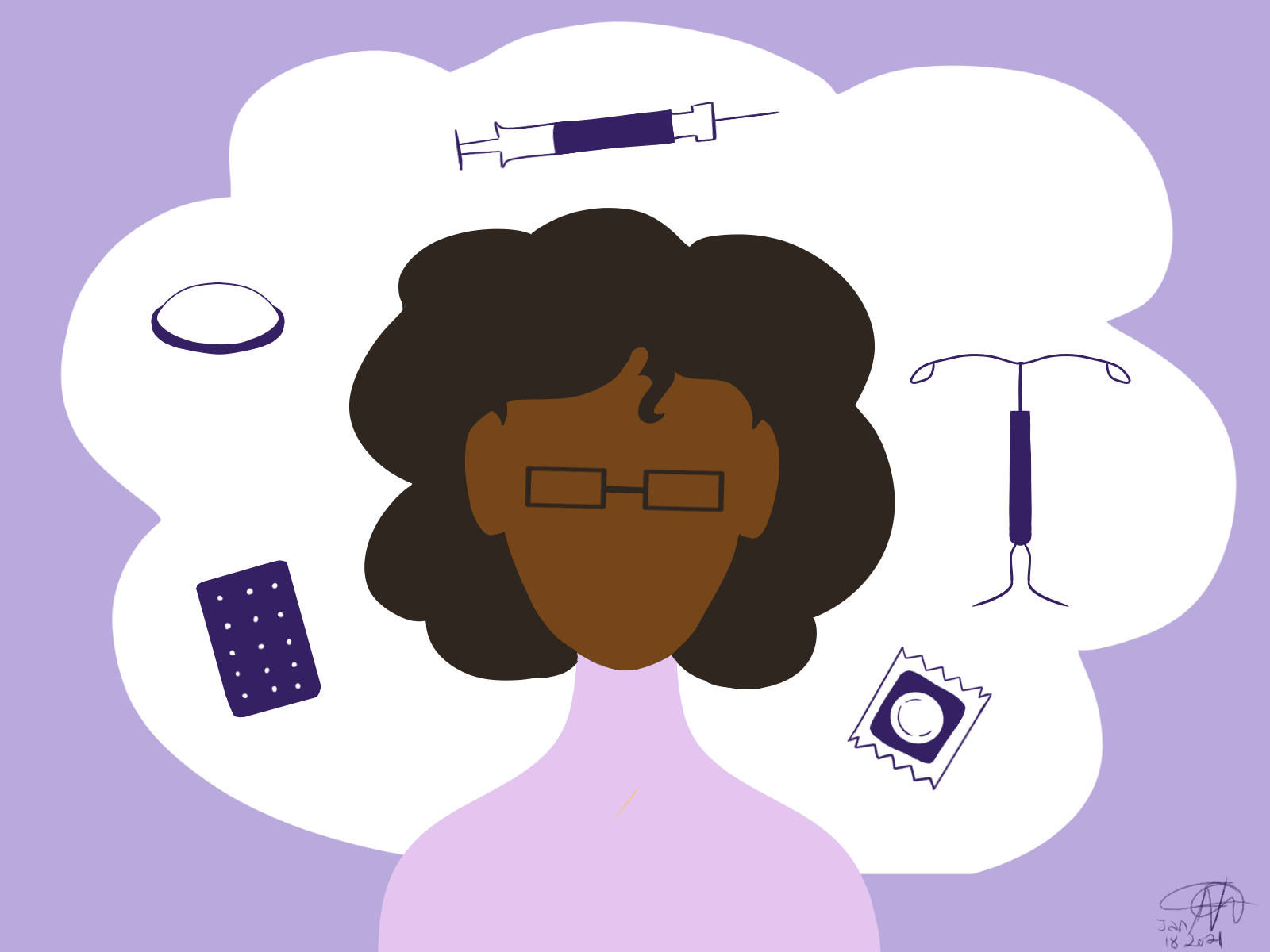
Why hadn’t Chantel considered an intrauterine devices (IUD), I wondered? Did she even know about them? Though they have been around since the time of the ancient Greeks, I myself had only become aware of the contemporary t-shaped version within the last 2-3 years. In conversations with other African women about birth control, I rarely hear IUDs mentioned. There’s a great deal about condoms (male and female), the Pill, the shot and postinor. Which – I should add – is emergency contraception, regularly misused in Ghana and is dangerously conflated with regular birth control.) I decided to investigate why this device was missing from African women’s arsenal of family planning/pregnancy prevention tools. What were our experiences like with this product? Here’s what some uterus owning people had to say:



OK… So not the feedback I was looking for, especially since I am considering getting an IUD for the exact opposite reasons (i.e. lighter/no periods), but these reports are consistent with much of the literature I found on IUD use among women of African descent.
WHAT IS THE APPEAL OF AN IUD?
IUDs are a type of long-acting reversible contraception (LARC). They are highly effective in preventing pregnancy. They last for several years and are easy to use. An annual checkup is recommended after insertion. They are a convenient form of “set and forget” birth control (BC).
ARE THERE OTHER BENEFITS BESIDES BC?
Yes. The Mirena IUD implantable contraceptive was found to be superior to oral contraceptives and non-hormonal drugs approved for the treatment of heavy menstrual bleeding in reducing the condition’s effect on quality of life. In some cases, it can eliminate menstrual bleeding, the potential of which TC and I were seduced by.
“The crazy part is that I’m queer and dating a woman so I wasn’t even trying to prevent pregnancy!” said TC, who just had her IUD removed this month. “It was just to get my periods back on schedule!”
Mirena has also been prescribed for women who are taking estrogen as their hormone replacement therapy.
WHO GETS PRESCRIBED AN IUD? THE RACE FACTOR
A fascinating study published by Tiffany Nicole Bell at Yale University reveals the impact of patient race and number of past sexual partners on clinical decisions to prescribe IUDs. She points to a recent study that showed low-income women found that Black women were significantly less likely than whites to receive the intrauterine device. Some studies have “proposed that providers might be less likely to offer certain effective contraceptive methods to minority women, due to their speculation that these women would increase their sexual risk-taking behavior (e.g. decrease their condom use, or increase the number of sexual occurrences and partners) and consequent risk for HIV and sexually transmitted infections (STIs) due to a perceived decrease in susceptibility to pregnancy with contraception.
These sentiments were echoed in a South Africa based study/trial that was terminated early due to “international concerns regarding a possible association between DMPA (injectable contraception) and HIV acquisition.”
Black women from low-income countries and/or social backgrounds are less likely to be candidates for IUDs. There is a direct line between the (perceived) class of the patient and access to this particular form of BC care.
WHAT ARE SOME OTHER FACTORS THAT AFFECT USE AMONG AFRICAN WOMEN?
Many women lack awareness of modern contraceptive methods, including IUDs. I only became aware of them in recent years. IUDs are not one of the more popularly advertised forms of BC.

Contributing to low-moderate IUD use is cost. As mentioned previously, it is a R2000 ($173) upfront tab for the device. That represents 10 days of wages for the average low skilled worker in South Africa. In the US, the cost is $2000, may be covered by ACA.
Access, availability and convenience play a role in utilization. As I discovered during my recent doctor’s visit, IUDs are not readily available. A prescription must be filled, taking anywhere from 1-6 days, requiring an additional scheduled doctor’s visit, preferably during the course of one’s period. Many women do not have the liberty or access to this kind of disposable time during the work week. Additionally, *data from UNFPA-Supplies surveys conducted in 17 Sub-Saharan African countries in 2015 show that 0–66% of facilities did not have the IUD in stock when surveyed, and 0–47% did not have the implant in stock (not shown); the medians were 26% and 19%, respectively. These data support the impression that shortages are more common for the IUD than for the implant.
Healthcare provider attitudes and skill have been shown to play a significant role in how (or if) the IUD gets administered. While injections can be delivered by lower-level paramedical staff, IUDs and other LARCs require the services of a trained OB/GYN, so as to minimize the potential for patient injury. As many women can attest to, provider’s personal morals and attitudes can (and frequently are) barriers to access of all types of BC, not just IUDs. While my doctor is very (maybe too?) passionate and encouraging on the subject, there have been many stories of women who have been refused access to care when age, class, religion, puritanical impositions, etc. on either side of the pharmaceutical counter come into play.
SO, WHAT’S NEXT?
In conclusion, after researching and writing this article, I have chickened out of getting an IUD. I will just bleed until the day the Universe deems it no longer necessary that I do so. I AM curious if anyone has any positive experiences with an IUD? If so, I know I speak on behalf of the whole community if you would share that in the comments! …Or if you have horror stories you feel can top these three, that’s cool too. 🙂







3 comments On Why Aren’t More African Women Using IUDs?
The following comment is posted on behalf of DD, who asked that I share her experience with our community:
I found out about IUDs from one of my best friends. I had never really looked into contraception at the time because the guy I was seeing before wouldn’t indulge the conversation. I should’ve researched on my own but I was in love and stupid. I know better now. I’m in a healthier relationship and we’re definitely not ready to have kids so I talked to my girlfriend about contraceptive and she recommended the IUD because she had installed hers and it seemed to be working for her. Little did I know it’d turn out to be one of the most traumatic experiences my body has ever been through. Not the effect of the IUD itself but just how callous the staff at Marie Stopes were with me.
All was fine when I got there but that changed quickly when I went into the nurse’s office to fill out forms. She seemed absentminded and just not there for it. I tried to ask questions and she would respond nonchalantly. I wasn’t too concerned because my friend had already explained most of it to me and I felt ready. A bit shaken, but ready. The next step was to undress and go get the IUD installed. I followed all their instructions. Got into the room, laid on the bed, legs wide open all ready for plenty discomfort but very little pain. Ha!
The insertion started almost painlessly but the further the nurse went the more painful it got. I really tried to be a big girl about it but chale, pain is pain. There were two other nurses in there with me. One was busily playing with her phone and the other casually conversing. No one paying attention to the fact that I had started crying and complaining about pain. The nurse rather got annoyed. I kept lifting my butt off the bed to ease the pain and she kept impatiently insisting I put it down. She was really upset. I felt like I was being a baby and making her work difficult in the midst of all that pain. One of the nurses took pity and held my hand while the other kept on with her conversation.
After what seemed like an hour of torment, the installation was complete but I was still in pain. Lots of it. I called my friend in tears and she was so surprised at my reaction. It wasn’t supposed to hurt this much. She texted a bunch of her other friends who had IUDs and they all said it went smoothly and they went about they normal schedules. So why was this happening to me?
Turns out, before the installation, the nurses were supposed to give me a suppository AND FORGOT! They forgot to give me my drugs and had the nerve to stand there and act like I was overreacting. That’s what upset me even more. No remorse. No sympathy. I felt judged the whole time. At some point, one nurse even said “well, if it hurts that bad, I should come for her to take it out”. What?!?! It was just a horrible experience. I managed to complain to the head nurse before I got the hell out of there. It’s been a year, everything seems to be working fine but everything time I think about having to go back to take it out, I get shivers. I don’t ever want to go through that again but alas, this shit can’t stay in my body forever. Sigh.
And there’s my horror story with IUDs. Will I recommend it? I doubt. Haven’t done so yet anyway.
Interesting read, one thing I did notice was there seems to be use of the term IUD to incorporate all the forms, when there is a distinction between which ones are non hormonal like the copper one and the hormonal one which can be the mirena one. I found this a bit confusing to read as I couldnt distinguish what sort of contraception each person was referring too.
I understand your confusion. When I visited my OB, she used the term “IUD” for both copper and hormone releasing devices. However, my research on the net made a distinction between the two.
I believe the respondents all used the hormone releasing IUD (i.e. Mirena).
Thanks for asking such a probing question!